Care Planning & Mental Illness
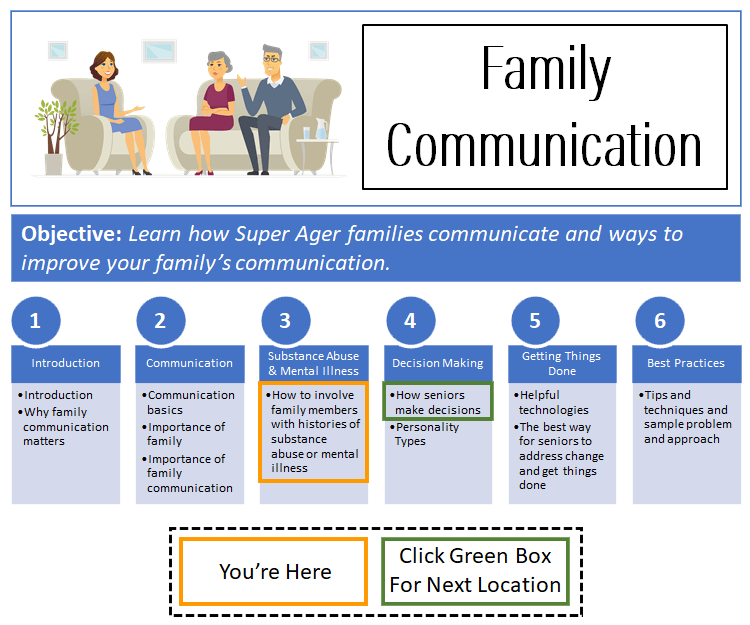
Click here to see what's on this page.
Carmena and I want to provide some comments on care planning and mental illness. This would also include care planning and alcoholism and drug addiction. Substance abuse and mental issues are also a very serious area of concern for anyone that examines how seniors and their families deal with aging-related issues.
Mental Illness & Substance Abuse Is Common
Almost every family has members that use and abuse drugs or alcohol. The same is true with mental illness. For example, alcohol use among Americans is estimated as high as 75 percent and the rate of “high-risk” drinking at 15 percent. High-risk drinking is having four or more drinks in a day for a woman and five or more for a man. Psychiatrists define problem drinking as alcohol use disorder (AUD). A recent detailed study determined that one in eight Americans are alcoholics.
Additionally, illicit drug use among Americans is estimated to be as high as 10 percent. That includes marijuana, prescription drugs, cocaine, hallucinogens, methamphetamines, and heroin. This statistic does not pick up seniors that may be using legal prescription drugs for inappropriate purposes.
Finally, the National Alliance on Mental Illness (NAMI) claims that 20 percent of Americans have or have suffered from mental illness. Mental illnesses also includes a number of disorders including anxiety, depression, post-traumatic stress, bipolar, and schizophrenia.
Risks Of Combining Cre Planning With Mental Illness & Substance Abuse
In our research, Carmen and I discovered something frightening. Because America has no framework or best practices for how families should address aging-related issues, families were unaware of the risks associated with alcohol, drugs and mental illness.
It’s Insidious & Ubiquitous
This might sound absurd, but it’s real. Here’s how it can happen. As parents, most of us are thrilled if our kids get into organized sports. Sports practices and games are supervised and coached. Kids are doing healthy activities. They learn to focus on goals and work together. The coaches teach them what they need to do every day to make those goals become reality. They learn that they get better results when they set goals and objectives. They learn life is about winning and losing.
But one in ten athletes uses performance-enhancing drugs. This statistic means on average, every high school athletic team has an illegal drug user. These drugs are dangerous under any conditions. Kids taking them unsupervised and in unmonitored quantities is especially dangerous. This reality means, one of our greatest thrills as an adult involves sending our kids to play with drug users.
Carmen and I get it. We all do our best to educate our children. But we really don’t take drug use by athletes all that seriously. We think we can manage our own children, that the coaches will keep any drug use away from our children or that the users keep their activities secret.
It Reaches Everywhere
The problem is that drug use affects behavior. That behavior can occur on the field or court. And that drug-induced behavior can and does cause injuries to others.
If you are reaching the conclusion that, that’s life, you are right. Our best defense is being diligent about trying to minimize the risks to our children and educating our children about the dangers and repercussions of drug use.
What Americans Know About Mental Illness & Care Planning
When it comes to aging issues and drugs, what have you been told? How have you been educated? What do you know about aging issues and mental illness? How have you been educated? We know nothing. Really.
Carmen and I discovered two suicides of family members deeply involved in their parent’s end-of-life issues. However, statistically we should have found none. Keep in mind that in most cases people don’t volunteer these tragedies. More often they hide these tragedies. Therefore, it’s possible there were more.
You might think the family members were unaware that this family member had mental issues. Wrong.
You also might think the family members were ignorant of mental health issues. Wrong.
You might also think the family members were estranged from one another and not actively involved in how people were participating in their parent’s end-of-life issues. Wrong.
The issue is very simple. No one has said what to do and not do relative to certain issues and end-of-life aging-related issues. No one has said, “Here are the best practices.” Please see our Best Practices below.
Family Members with Substance Abuse and Mental Health Issues Often Want To Help
Let’s say something upfront. Family members with substance abuse and mental health issues, and histories, are often brilliant, capable, compassionate, and earnest. This issue is not the people. The issue is the illness. The disease affects how people behave.
Mental Health & Substance Abuse Issues Mix Poorly With Care Planning
Care planning and mental illness don’t mix well. For example, studies show that under prolonged periods of stress and anxiety, people with substance abuse and mental illness perform poorly. Their ability to deal efficaciously with the realities of the external world erodes. End-of-life aging issues are always emotionally charged. Carmen and I describe them as hyper-emotional. People have trouble separating what the Ager is experiencing and wants from what they experience and want. Therefore, aging-related issues can easily become triggers, even for those that have not had any recent symptoms of substance abuse or mental illness.
Consequently, their ability to calmly, rationally, and honestly interact with family members is low. Even if the individual with the substance abuse or mental illness history is 100% recovered, it’s unlikely all the family members will have enough trust and confidence in the person to place them in charge where the position (1) involves high stress, (2) requires high competency, and (3) decisions affect other family members. A person that is really 100% recovered will understand this reality.
Here’s How People With Mental Health & Substance Abuse Issues Can Help
However, this doesn’t mean the person can’t help and participate in aging-related issues. If it makes sense for your family, and it often does, they absolutely should participate and be invited to participate. It is how you mix care planning and mental illness that matters. The same is also true for care planning and substance abuse. We will address this in the best practice section below.
There are also situations when someone with mental illness and substance abuse should not participate with families addressing aging issues. That’s a family issue to be addressed.
Carmen and I want to help families that decide to involve family members with mental illness and substance abuse histories by offering a framework for inclusion. See the best practice section below.
For example, Carmen and I discovered family members with mental health issues and substance abuse issues and histories were most involved in a few common areas.
Sharing Their Expertise
Firstly, we noticed family members with specialized expertise often taking control of those areas. Common areas included:
Health
Family members with specialized medical skills often took charge of their areas of expetise.
– Doctors
– Nursing
– Rehabilitative therapies
Finances
Financial experts also took charge of their areas of expertise.
– Money management
– Bill paying
– Budgeting
– Tracking spending
Sharing Their Religion/Beliefs
We also noticed very religious family members liked to help Agers with strong religious commitments. For example, we found family members that had dealt with substance abuse or mental illness reconnecting or turning to faith to help address issues or stay disease-free. Once committed to the Church, they were eager to help Agers continue or begin their participation.
> Attending Church (e.g., Synagogues, etc.)
> Staying active in faith-based social and outreach programs
Care Giving
The last area we found family members with substance abuse and mental illness issues or histories interacting with Agers was caregiving. Frequently a person dealing with substance abuse or mental health issues, or in recovery, had trouble finding a job or needed a place to live. A parent’s or grandparent’s home was often a safe haven in this time of need. Caregiving was often traded for the free room and board. Common areas included:
> Living with an Ager
> Taking an Ager to medical appointments
> Helping with ADLs (toileting, eating, etc.)
> Helping with IADLs (bill paying, shopping, cooking, cleaning, etc.)
In every case above, when the family member has mental issues or substance abuse issues, it’s important to minimize the street of making decisions. Never place someone with these conditions in charge of making decisions alone. It’s often too much.
Best Practices for Family Members with Substance Abuse and Mental Health Issues
Carmen and I want to help families that decide to involve family members with mental illness and substance abuse histories in aging issues. In other words, we want to offer best practices. The framework below may help.
T-O-G-E-T-H-E-R
The basic rule Carmen and I want to communicate is T-O-G-E-T-H-E-R. Use TOGETHER as a framework for working with family members with a current or historic issue with substance abuse or mental illness.
CarePlanIt created an acronym called TOGETHER. It informs and emphasizes best practices for dealing with age-related issues that are being dealt with by family members with histories of substance abuse and mental illness.
TOGETHER means at its heart the activity, task, endeavor is done with a group of people. There is no one person fully in charge. The stressors of many end-of-life aging issues are too great for someone with a history of certain diseased. The risks are too great to allow that one person to stand alone.
For discussing the acronym, we’ll use Rita, as the family member with a history or substance abuse or mental illness. Rita has recovered, or is in recovery.
T – Trust:
No one in recovery wants to be distrusted. People in recovery want trust. They understand their historic behaviors have been untrustworthy, but they are now in recovery and their actions are now trustworthy. So give the person some trust. Give Rita some slack to make decisions and operate independently.
O – Observe:
Observe means that someone must observe the interactions between Rita and the Ager. Other people must observe the actions between Rita and the Ager. If Rita is paying bills, these transactions review online. In fact, it makes sense to pay all bills online. If Rita is living with the Ager, someone should periodically drop in and see how everything is going.
G – Gather Information:
People other than Rita should gather information helpful to Rita and the Ager. If Rita is paying bills, find the online options available and offer Rita that information and help setting it up and even taking over the payment process if she wants.
E – Enjoy:
Aging-related issues are laborious, time-consuming and frustrating. Enjoy whenever you can. Celebrate Rita and her efforts. Let Rita know it’s OK to enjoy.
T – Talk:
Communication is critical. Talk on some kind of schedule that Rita and the family agree on. It doesn’t have to be every day or week. Figure out what makes Rita and the family comfortable.
H – Help:
Provide Rita with help. We’re not talking respite type help yet, we’re talking help. The number one issue family Caregivers have is that other family members don’t help enough.
E – Employ:
Consider what Rita does as employment. She is a kind of employee. Should she be paid? The family should certainly calculate what the work Rita is providing would be worth if it was purchased from a non-family member. What is done with this information is a family issue.
R – Respite:
Respite care is relief for Rita. This isn’t help from family. This is scheduled and if necessary, paid for help so Rita can take a vacation from the Ager. If Rita is spending hundreds of hours a month with the Ager, respite care should be provided.
Always Avoid Hyper-Charged Circumstances
A final best practice note:
Never place a person with a current or historical mental illness or substance abuse issue in charge of hyper-charged aging-related processes or issues.
These include:
This doesn’t mean they can’t participate. Just don’t make them the point person or the primary decision-maker. In other words, TOGETHER, never alone.
NOTE: Mental health and substance abuse problems are very serious. Consequently, we always encourage families to involve professional mental health and substance abuse experts to help navigate any emotionally charged issue.
Other Resources On Care Giving & Mental Health
A good resource on mental health issues here.
Make sure to see our other sections, especially, Getting Things Done here, and Best Practices: Tips and Techniques, here.