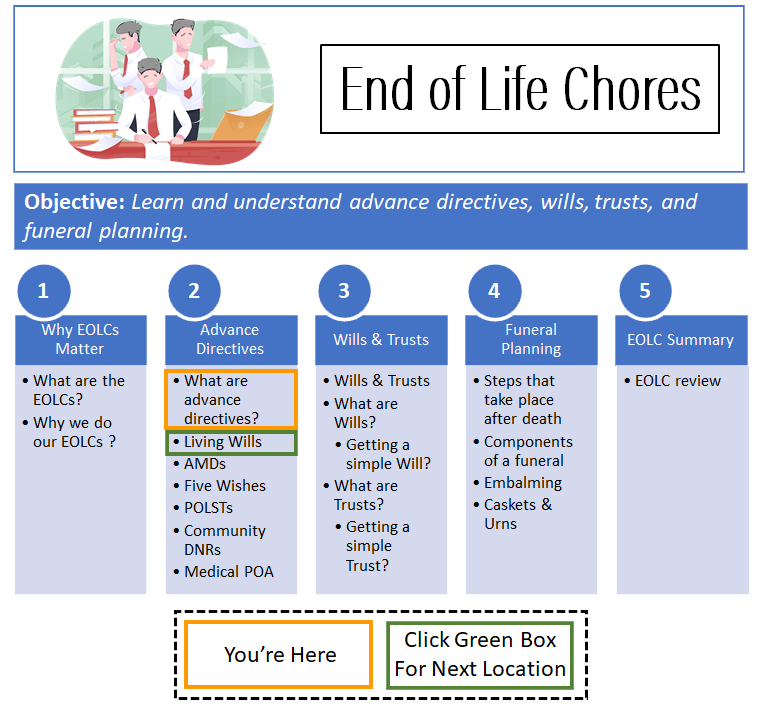
Advance Directive Documents
Click here to see what's on this page.
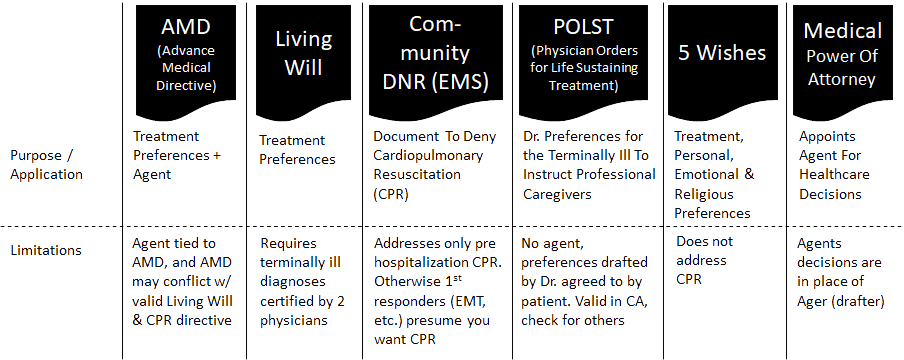
Advance directive documents come in many forms and flavors. However, there are six major ones seniors should know about. These are:
Many do the same or similar things, others are unique. See the chart below for a quick overview of these advance directive documents.
Origins Of The Living Will
Living Wills have the earliest origins in the life-sustaining medical treatment world. They were first proposed by lawyer Luis Kutner to allow a terminally ill or dying person to express their wishes regarding medical treatments. It addressed the growing issue of how an incapacitated and terminally ill patient’s life is prolonged with medical treatments.
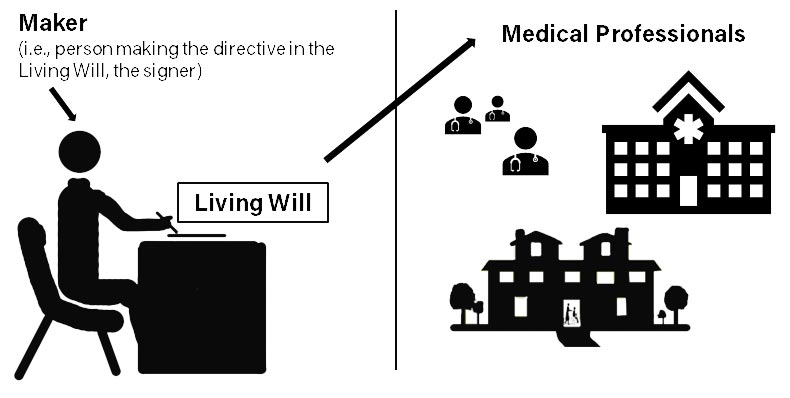
A maker (creator) drafts a Living Will (LW) so that medical professionals can provide only the life-sustaining medical treatments the maker wants.
Kutner also had a deep appreciation of what a bad death, an inappropriately prolonged life could mean. For example, he said, “[t]he Living Will premise is that prolongation of the dying process by tubes and supportive machines of modern hospitals is desperately barbaric.” Consequently, the goal was to allow the patient to choose what treatments they wanted in order to reduce prolonging a painful and poor-quality life.
Kutner and supporters enlisted State legislatures to adopt state Living Will statutes and model documents. They also had a broad swath of constituents that were encouraging them to act. Doctors and hospitals were trained to treat people and keep them alive. However, there were legal issues involved if they failed to treat, and worse implications if they withdrew treatment. Friends and family of patients in comas or vegetative states were also supportive. In other words, they were desperate to address what they were witnessing.
Institutionalization Of The Living Will
States jumped on the bandwagon during the 1970’s. Even the Catholic Church got on board by dropping any opposition to Living Wills in 1984. The majority of State now had Living Will Statutes. In 1985 the National Conference of Commissioners on Uniform State Laws adopted the Uniform Rights of the Terminally Ill Act (UTRIA) in an effort to make it easier for people to create Living Wills and have confidence that other States would honor these documents.
Living Wills focused on patients (1) diagnosed with terminal conditions and (2) unable to make their wishes for treatment known. By definition, this required Doctors to certify that a patient was both terminal and unable to express their current wishes. In other words, it was conditional.
UTRIA and its iterations codified best practice definitions for key areas of Living Wills like “Life-sustaining treatment,” “attending physician,” and “terminal illness.” It also created strong immunity provisions for physicians and hospitals.
Despite Codification, Problems In Interpretation Linger
But even the codification of best practices and its adoption by states did not make the language and definitions fool proof. For example, some families argued that the doctors were wrong about the terminal diagnosis. Or that the patient had communicated a desire to change their wishes. This created some problems.
While the Living Will statutes and best practices from UTRIA were working their way through state legislatures, the federal government started making it clear they wanted Living Wills required on admission from facilities receiving federal funds via Medicaid and Medicare programs.
Administrators of Medicare and Medicaid recognized that 20% – 40% of their expenditures were used on services during the last couple years of their beneficiary’s life. These services were probably unwanted or unwarranted treatments that a Living Will would avoid. The federal government began requiring facilities (nursing homes, hospitals, etc.) to get a patient’s Living Wills (or Advance Medical Directives) in order to get reimbursed. In turn, these facilities began requiring their patients to complete or submit a Living Will (or Advance Directive) on admission.
All States Have Living Wills, Here’s How To Find Yours
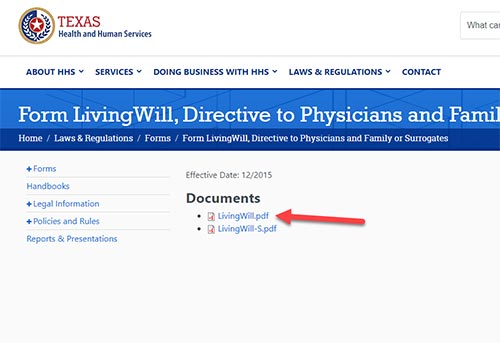
All this effort resulted in every state adopting some form of Living Will. To find what your state uses, type into Google (or another search engine) your state and Living Will. You’ll get your state’s Living Will form. However, to be valid you need to fill it out, sign it and have it notarized or witnessed.
Step 1:
Type your state and Living Will into a search engine.

Step 2:
In the results, look for the URLs with a “.gov” extensions.
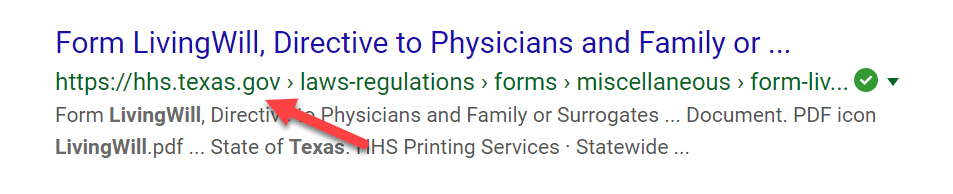
Step 3:
Find the Living Will form on the government site.
The document, however, may be titled Living Will or Advance Medical Directive. This is a good segue into the differences between Living Wills and Advance Directives. Originally, a Living Will had no Agent provision: a provision where the maker appoints a person to make medical decisions on their behalf. The Living Will concept didn’t require an Agent. Instead, the provisions defined key areas like “terminal illness,” “life-sustaining treatment,” “attending physician,” and “irreversible condition.” The maker would sign the form and the “attending physician” would essentially certify that the provisions in the Living Will (e.g., terminal illness, irreversible condition, etc.) are met.
Weaknesses Of Living Wills
Living Wills quickly came under attack for things like vague language. What did “irreversible condition” really mean? What was a “terminal illness?” Critics also found issues with “life-sustaining treatments.” What exactly was life-sustaining? How would new technologies fit into this definition? Family members asked why the “attending physician” was the one making the decision. What if a family member thought there was a better physician to make the decision or that they should make the decision because they knew the maker better than any physician.
Strengthening Living Wills
One quick way to address many of these issues was to add to the Living Will form a medical power of appointment provision enabling the maker to name an agent to make medical decisions. By appointing an agent, the maker could select someone that knew them well and understood their desires concerning life-sustaining and life-prolonging medical treatments. This agent could, in theory, consider everything the maker would have considered.
Once the agent provisions were being tossed around in became clear, the Living Will was more than a narrowly tailored document. It was becoming more like an “Advance Directive.” An effort for the maker to direct their future goals and desires for medical treatments.
Today, the names are often used interchangeably. But a traditional Living Will is likely to omit a provision allowing the maker to appoint a medical decision maker, whereas an advance directive will generally include a provision to name an agent for medical decisions.
Origins Of The Power Of Attorney
Another form of the advance directive document is the Power of Attorney. Since we’re on power of attorneys (POA) let’s go to this document. POAs have been around for thousands of years. They are documents that allow an individual to act on another’s behalf. Think about how a merchant with a shop in the center of a City would conduct simultaneous business at a port a hundred miles away. The merchant couldn’t be in two places at one time, so he would appoint an agent to act on his behalf. He would sign a document authorizing another to act of his behalf transacting business at the port.
The Medical Power Of Attorney
In the medical domain, POAs are called a Medical Power of Attorney. A Medical POA appoints another to make your health decisions. Most medical POAs are conditional. Conditioned on the need for the maker to become incompetent. This generally meant the maker is unconscious or clearly incompetent. This is not always a black and white question.
Five Wishes
Another form of the advance directive document is Five Wishes. Five Wishes (see fivewishes.org) was created by Jim Towey. Mr. Towey spent time in a home where people were facing terminal illnesses. It was clear that people facing death had wishes in other areas. Five Wishes tries to pick up some of these and incorporate them into a single document. They include the desired life-sustaining medical treatments and an appointed agent. They are unique because they also add wishes from other domains.
The Five Wishes website says,
Five Wishes is unique among all other living will and health agent forms because it speaks to all of a person’s needs: medical, personal, emotional and spiritual. Five Wishes also helps to guide and structure discussions with your family and physician, making conversations easier.
Five Wishes is an easy-to-use legal advance directive document written in everyday language. It helps all adults, regardless of age or health, to consider and document how they want to be cared for at the end of life. It is America’s most popular living will with more than 35 million copies in circulation.
Five Wishes actually qualifies as a valid Advance Directive in 42 states, according to their website. With some minor modifications and adds, the document can meet every state’s requirement.
Drawbacks Of Living Wills, Advance Medical Directives, Medical Power of Attorneys, and Five Wishes
Living Wills, Advance Medical Directives, Medical Power of Attorneys and Five Wishes all had one drawback: a clear way to communicate to first responders and emergency room personnel. In other words, how do you let first responders know the wishes of the patient when someone collapses, gasps for breath or appears non-responsive.
For example, unless the AMD, LW or POA (with the appointed agent) show up with the patient, it’s unlikely the patient’s wishes will be followed. Even if they show up with the patient, the emergency team is likely to kick into gear to save the patient versus trying to interpret the document or verify that the agent is the agent. These are also first responders trained as first responders, not as lawyers or medical administrators.
POLSTs & DNRs
POLSTs
Other forms of the advance directive documents are POLSTs and Community DNRs. The major difference between Physician Orders for Life-Sustaining Treatment (POLST) and the documents discusses above is that a POLST is signed by a licensed physician. It’s also a document recommended for seriously ill patients. It is unlikely a physician would sign a POLST for anyone other than a terminally ill patient. A POLST is not a form that a state legislature has to approve. It is a legally recognized document that you and your physician discuss and sign.
For example, physicians, hospitals and health groups can use POLSTs as part of their regular standard of care. Because it’s signed by a physician and filed in the patient’s chart it becomes a standing medical order. The same way you’d look at the patient’s chart to find their allergies and treat them with this knowledge is the same way you’d find a POLST and treat with this knowledge. It’s also portable across providers and state lines.
Most important, POLST as standing medical orders do not require a patient to be incapacitated for it to take effect. There are some state to state restrictions, so you need to check the state you’re in to see if it recognizes the POLST’s of another state. But if your health provider recognizes POLSTs, and most do, they are likely to honor the POLSTs wherever they are providing, and often paying for, medical services. POLSTs are considered medical instructions for emergency medical personnel. This includes first responders. However, in an out of hospital situation where a patient chart may be temporarily unavailable, even POLSTs may be unfollowed at the point of service.
Community DNRs
Also, think of this emergency. The fire department, for example, gets a call from a skilled nursing home or private home requesting emergency medical services (EMS). EMS teams are composed of emergency medical technicians or paramedics. Paramedics are also trained in advanced life support (ALS). These include for example, endotracheal intubation and IV support. EMS teams are also staffed by lesser training responders called emergency medical technicians (EMT). Both EMT and Paramedics can provide CPR.
The EMS team is also trained to keep patients alive. In other words, if they show up and the patient is having trouble breathing or is non-responsive, what do they do? Unless they have also called the hospital and the hospital has identified an advance directive and interpreted it as applying to this situation, the EMS team will do what they’re trained to do. In other words, they keep the patient alive.
The state of California and a few others have created the ability to recognize POLSTs and what’s called a Community Do Not Resuscitate (DNR). A licensed facility (e.g., nursing home, skilled nursing home, hospice, etc.) with a POLST or DNR form on file will hand that form to the EMS team. EMS teams are also trained in states that recognize POLSTs and Community DNRs to respond based on the information on that form.
Moreover, even outside of a licensed facility, handing an EMS team a Community DNR or POLST will usually tie the EMS team to that form. In some states, they also recognize bracelets or medallions worn by the patient.
Miscellaneous Issues
Finally, the documents above are designed to assist incapacitated people to make their medical treatment wishes known. But anyone that’s ever worked with people facing terminal illness or advanced old age knows that these people have wishes in more dimensions than those in life-sustaining medical treatments. However, five wishes address some of these other domains.
In other words, at the big picture level, a broadly encompassing directive is very helpful.
Other Resources On Advance Directive Documents
Yous can also learn the details about these directives in these other Sections: advanced medical directives here, living wills here, community DNRs here, physician orders for life sustaining treatment here, five wishes here, and medical power of attorneys here.
A good resource on advance directive documents from the National Institute on Aging is here.