Alzheimer’s Disease (AD)
Click here to see what's on this page.
Alzheimer’s is an illness category under the umbrella disease of dementia. It’s the most common form of dementia. It is progressive and incurable. Symptoms often progress from memory loss to the inability to carry on a conversation to the inability to respond to the environment. Alzheimer’s affects the parts of the brain that mediate and manage thought, memory, and language. As we age the chances of getting Alzheimer’s increase. Twenty-one percent (21%) of women over the age of 65 will develop Alzheimer’s. Twelve percent (12%) of men over the age of 65 will develop Alzheimer’s.

Consequently, one in three seniors dies with Alzheimer’s or another form of dementia. These diseases cost Americans $355 billion each year. More than 11 million American’s provide unpaid dementia care to family and friends. Billions more are provided by paid professionals. In sum, Alzheimer’s Disease is one of the greatest threats faced by America’s aging population.
Also, see our page on dementia.
Alzheimer’s Phases
Alzheimer’s is now being viewed in two general phases. There is a preclinical phase, where the disease is identifiable but does not impair daily functioning, and a clinical phase where daily functioning is impaired.
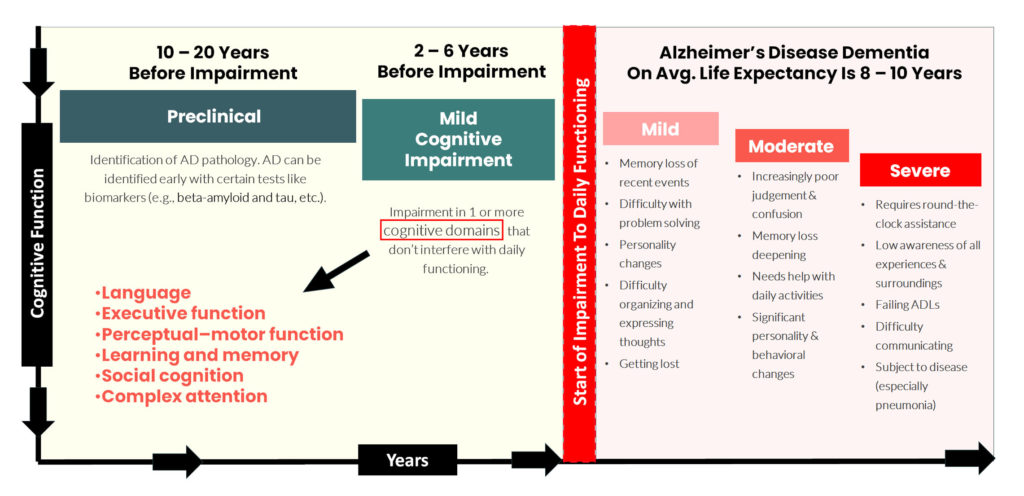
Alzheimer’s Preclinical And Mild Cognitive Impairment Phases
This phase of Alzheimer’s disease starts 10 – 25 years prior to any impairment in daily functioning. Preclinical AD is defined when the AD is likely starting in a patient but diagnosis is difficult if not impossible. Family history is often an indicator of patients at risk.
There is also a part of this phase called mild cognitive impairment where there is some cognitive impairment but no impact on the individual’s daily functioning. At this time doctors can discover evidence of AD pathology (test identifies AD markers) but there are no clinical symptoms. These markers can be identified 2 to 3 years prior to any symptoms.
Tests that can identify amyloid beta (Aβ) can diagnose AD. Tests that can do this include positron emission tomography (PET) imaging and cerebrospinal fluid (CSF) tests. For a more detailed explanation see this page from Biogen.
During the mild cognitive impairment phase, there is some cognitive impairment but no impact on the individual’s daily functioning. Psychiatrists look at cognition as consisting of a number of domains. Impairments can emerge in any one or combination of these domains. These generally include the following:
If just one domain is impaired, its usually does not have a severe impact on daily living.
How Preclinical and Mild Cognitive Alzheimer’s Impact ADLS and IADLS
Thus, by definition, seniors’ activities of daily living, and instrumental activities of daily living are not impacted. Once they are, AD moves into the next phase. See explanations of ADL and IADLs here.
Alzheimer’s Disease In Seniors
At a certain point, a person subject to Alzheimer’s disease has their disease impair daily functioning. There are three stages at this point: mild dementia due to Alzheimer’s disease, moderate dementia due to Alzheimer’s disease, and severe dementia due to Alzheimer’s disease.
Mild Dementia Due to Alzheimer’s Disease
When AD impacts a senior’s daily functioning, the disease is classified as mild dementia due to Alzheimer’s disease.
At this stage, symptoms include
How Mild Dementia Due to AD Impacts ADLs and IADLS
Sufferers have increasing problems with IADLS and ADLs. At a minimum caregivers should look over the shoulder of sufferers. For example, caregivers or family members can start to review bill paying and check writing. They can identify and ensure payments are made on insurance policies (car, home, health, etc.). Accordingly, one of the easiest ways for this is for the caregiver to gain access to the sufferer’s bank and brokerage accounts. Online access is the easiest. However, if the caregiver is not a co-owner of the accounts, legally, a power of attorney should be created. See our section on POAs here. If the impact to the sufferer’s life is severe, a family member or caregiver may be best be positioned to take over these responsibilities.
Moderate Dementia Due to Alzheimer’s Disease
The signs of this stage of the disease include:
How Mild Dementia Due to AD Impacts ADLs and IADLS
Once you’re in the middle of AD the ability to competently perform IADLs is gone. Others will need to shop, cook, bank, and manage medication for the sufferer. It’s also likely the sufferer will need help with ADLs.
Severe Dementia Due to Alzheimer’s Disease
The signs of this stage of the disease include:
Progression rates for Alzheimer’s disease vary widely. On average, the average lifespan post-diagnosis is between 3 and 11 years after diagnosis. However, some survive 20 years or more. The degree of impairment at diagnosis can affect life expectancy. AD progression is faster in cases where vascular risk factors such as hypertension are untreated.
How Severe Dementia Due to AD Impacts ADLs and IADLS
An individual with severe AD needs help with most or all of their ADLs. Therefore, family, finances, and housing become critical areas to assess.
Great references for Alzeimer’s Disease
Center for Disease Control – https://www.cdc.gov/
Mayo Clinic – https://www.mayoclinic.org/
Alzheimer’s Foundation – https://alzfdn.org
CarePlanIt’s Approach
CarePlanIt classifies every issue into one of five key areas: health, housing, finances, end-of-life chores & family communication. Once done, the CarePlanIt framework allows you to create an optimized process of addressing the challenge. You minimize your family’s time and costs while maximizing your chance at reaching an ideal solution. Although all five categories work together, it’s important to make an initial categorization.
Alzheimer’s Disease Is A Health Issue
Alzheimer’s is a “Health” issue. The disease is horrifying and frightening for the patient, family, and caregivers. But CarePlanIt can help you better understand the impact of Alzheimer’s on your life. Generally, for Health related issues, CarePlanIt helps you optimize your finances, identify how your disease impacts your needs, and optimize your family’s participation. Furthermore, Alzheimer’s impacts a sufferer’s ability to perform ADLs and IADLSs. Review them here.
Alzheimer’s Disease Is A Housing Issue
Moreover, Alzheimer’s Disease quickly becomes a housing issue. For details, see our Section on Housing. There are only three ways to live: independent, assisted, or dependent. For this reason, CarePlanIt can show you how to easily navigate issues relating to the need for assisted living/dementia care (assisted) or nursing care (dependent).
In short, someone with Alzheimer’s is likely to require continuous supervision. This can be provided by:
As a result, depending on your area, a private in-home caregiver can run between $10.00 and $25.00 an hour. If you look at help for $10 an hour, for 8 hours a week, five days a week, you’d spend $21,000 a year. At $25 an hour, for 16 hours a day, seven days a week, you’d spend $125,000 a year.
Similarly, depending on your area, assisted living for an Alzheimer’s patient can run between $5,000 and $10,000 a month or $60,000 to $120,000 a year. Nursing home care can run between $6,000 and $12,000 a month, or $72,000 to $144,000 a year.
Quick Ideas From CarePlanIt
Managing the costs of supervising an Alzheimer’s patient is often a family’s major challenge. Hence, family cooperation is critical. Here’s what many families do: